The Impact of Online Video Learning Activities on Nurses’ and Midwives’ Continuing Professional Education by Anne Wilson in COJ Nursing & Healthcare_journal of nursing and healthcare impact factor
Abstract
Highlights
New knowledge/skills from CPD provides increased confidence to
advocate for best practice; New knowledge/skills result in improved
selfefficacy
enabling better patient care and better patient education; CPD fosters
leadership skills and confidence in demonstrating influence on
health outcomes; The benefit of continuing professional education in
improving competence is identified; The major benefits of online
learning are
convenience and increase accessibility to education
‘This study was conducted to determine the effects of continuing
professional development via online Video Learning Activities for nurses
and
midwives and the perceived contribution to their practice. Change in
knowledge, skills and self-efficacy due to undertaking online Video
Learning
Activities was assessed by two online questionnaires applied through
Survey Monkey TM. Forty-two online learners entered the study and 36
(85.7%)
participants completed the entire protocol. Our study demonstrates
supports the use of innovative Video Learning Activities as part of
continuing
professional education to expand knowledge and skill [1], promote
positive attitudes among nurses and midwives, strengthen patient
provider
relationships, and enhance well-being. Online learning via Video
Learning Activities resulted in the acquisition of new knowledge and/or
skills.
Learning outcomes included change in clinical practice, management
practice, workplace culture, increased awareness of patients’ rights,
and improved
communications with colleagues.
Keyword: Continuing professional education; Video learning activities; Electronic learning; online courses; Survey
Introduction
Nurses and midwives are commonly parents, spouses, and
carers and are working in addition to studying. There is considerable
demand on their time and their responsibilities are high. Hence,
they need flexible study options that are relevant and accessible at
times and in locations that suit them [2]. All these factors impact
on their choice of learning program. Factors nurses and midwives
may consider when choosing the right e-learning provider include;
type of program, type of delivery, the subject material offered [3],
currency of material, how it is offered, when it is offered, where it
is provided, who offers it, who recognises it and being able to move
through it at their own pace.
Online learning as an educational tool for professional learning
and continuing professional development (CPD) has developed
relatively quickly and expansively [3]. Accordingly, the number
of continuing education initiatives that are offered in electronic
formats for the health professions has grown exponentially [4]
and does not appear to be abating [4]. In response to the demand
for time efficiency, and encouraged by intensive competition and
globalization, learning enhanced by information technologies
has gained momentum [5]. This is partially as people’s lives have
become increasingly mobile, complex and multi-dimensional,
online learning has made access to education more accessible,
affordable and desirable. People frequently work in changeable jobs
or situations that require new skills or may cause them to travel
or relocate. Nurses and midwives are a prime example as they are
frequently shift workers, move in a trajectory from novice to expert
and may work in rural or remote areas or be located abroad.
Online learning can be defined as the use of electronic media and
information and communication technologies (ICT) in education
and may be referred to, among other terms, as E-learning. As such
distance education and learning has developed to encompass
sophisticated innovations in content delivery [5,6]. Broadly, it is
delivered digitally through numerous online mechanisms that
include text, audio, images, animation, and streaming video.
Online video tutorials addressing specific knowledge points
are recognised as valuable, flexible, and cost-effective tools that
improve users’ knowledge, skills and self-efficacy [7,8]. Whilst some
consider online learning may never be a complete replacement for
live classroom instruction, there are unique ways to use technology
to assist student learning [6]. Online video tutorials offer targeted
lessons designed with one specific learning goal, as opposed
to presenting learners with broad course instruction or larger
concepts digitally that they must filter through without being able
to ask questions.
The adoption of technology in the provision of education has
been extremely important in providing up-to-date, contemporary
information to meet learners’ needs. The development of the
internet has enabled education providers to modify their approach
and serve students in much better and more creative ways [9].
Online video learning provides learners with increased flexibility
in terms of time and place of study in addition to how much time
they need to spend on a specific topic [9], depending on their prior
knowledge. An advantage [7], when an area of learning difficulty
is encountered, learners are able to view the tutorial material
several times until they fully understand; and, for other points on
which they are familiar, they can skip parts of the tutorial if they
are comfortable with the knowledge point. Thus, video tutorials are
learner controlled, need-based, and task-oriented learning aids.
There is some literature that reports the effect of Internetdelivered
continuing education on changes in knowledge, skills, and
self-efficacy on health professional education (Martin, Bruskiewitz,
& Chewning, 2010). Self-efficacy and perceived ability to counsel
patients on healthy behaviour has been known to improve
significantly after CPE [10]. Nurses, midwives and other regulated
health professionals must be confident that the e-education they
access is current, relevant, and of a high standard, facilitating
their professional and legislative requirements. Registered health
professionals such as nurses are required to undertake CPD to
maintain their registration to practice and need education that is
theoretical, informed, rigorous, and meets registration standards.
A wide variety of different types of online education services
are available and as they are continuously evolving, it is crucial
that their effectiveness for the learners’ needs and for the safety of
the community that sustainable and quality services are ensured.
If optimum knowledge transfer to learners is to occur, monitoring
performance and outcomes of education programs requires
evaluations and appraisals that keep pace with the rapid changes in
learning technology and learners’ needs. This is also an important
requirement for education providers seeking accreditation of their
programs [9]. The purpose of this study was to determine the
effects of online video learning activities in delivering educational
activities that improved learners’ self-efficacy, knowledge, skills
and that this new knowledge was, in some way, translated into
practice.
Methods
A nursing education and technology company based in North
Melbourne Australia, and specializing in web-based technological
applications that help nurses with continuing professional
development, commissioned an independent consultant to
evaluate users’ perceived effectiveness of VLAs provided by its
online ‘Learning Centre’ on their professional development.
Effectiveness is self-reported to indicate effects on learners’ selfefficacy,
knowledge and translation of knowledge into practice.
Permission to conduct the study was provided by the Belberry
Human Research Ethics Committee. A descriptive exploratory
design involving two phases of data collection via two online surveys
was undertaken. Both numerical and text data were collected and
statistical and text analyses applied.
Theoretical framework
A descriptive, exploratory survey design was used to identify
users’ perceptions of the educational benefit of their learning
experience and to indicate its effects on processes and outcomes
of clinical care. The survey tool utilised a mixed method evaluation
approach of quantitative and qualitative questions. Questionnaires
were formulated based on studies retrieved from the reviewed
literature, the research question and the knowledge of the research
team. In particular, the data collections tools were informed
from those described by Carlson [11] and England [7]. Although
published instruments had been used, both questionnaires were
pre-tested prior to their application to ensure validity and reliability
in the existing population.
Measures
Questionnaire one sought personal and professional
information, how participants anticipated translating their new
knowledge and/or skills into practice, and the impact of VLAs on
knowledge, attitudes and skills. Questionnaire two investigated
whether the VLA resulted in new knowledge and/or skills and if this
had an impact on certain areas of practice; and how respondents
translated their new knowledge and/or skills into practice. Openended
response opportunities invited participants’ to elaborate on
their responses after most questions in both questionnaires.
Sample
Online subscribers who completed a VLA through the ‘Learning
Centre’ during the data collection period and who indicated in
their evaluation that they planned to use their learning to make
improvements to their practice were identified and invited to
participate in the study. A letter detailing the purpose, intentions,
and requirements of participation and link to the first questionnaire
was emailed by the investigator to identified participants. At the end
of the first questionnaire, participants were asked to provide their
email address if they consented to being contacted to participate in
the second questionnaire. The setting for the study was in the online
environment at personal computers of participants’ choosing.
Procedures
The two questionnaires were applied online through Survey
Monkey TM two months apart. Questionnaire one opened on
15th May 2014. The participant information sheet and a link
to the questionnaire on Survey Monkey TM were sent to online
subscribers who indicated that they would use their learning from a VLA
completed during 14th April 2014 to 13th May 2014 to make
improvements to their practice. Participants were given three
weeks to complete the survey and a reminder email was sent at the
end of the second week.
The link to the second questionnaire was sent via email to 36
out of 42 participants who responded to the first questionnaire
and provided their consent and email addresses to be contacted.
This email was sent on the 15thAugust 2014 and participants were
advised they would have three weeks to complete the survey. A
reminder email was sent one week before the due date.
Data Analysis
Participants’ responses were analysed with descriptive
(summative, frequency and percentage) statistics, and reported
in tables, charts and free text. Data were imported from Survey
Monkey TM for management in Excel TM and checked for accuracy
and quality. Descriptive statistics were used to characterise the
sample. Liker response data was analysed to report the most
frequent response with the spread of responses displayed in
charts/graphics.
Textual data were entered into a word document for each
question. A content analysis was then conducted on the data
with the responses grouped according to the meaning, or overall
sentiment, of the response [12]. Where some responses provided
more than one meaning, the response was counted towards each.
Results
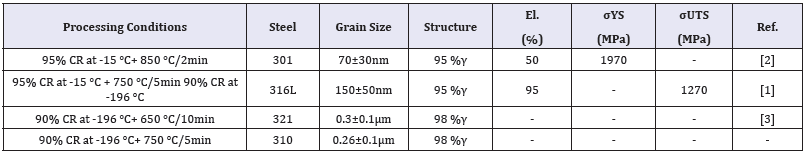
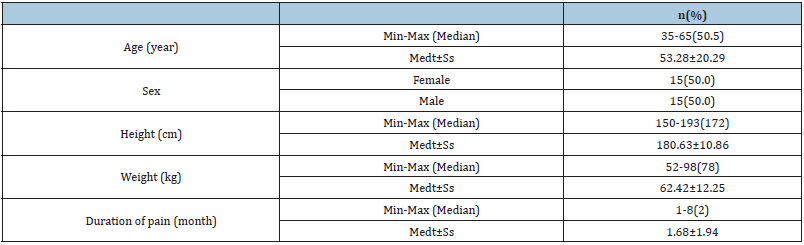
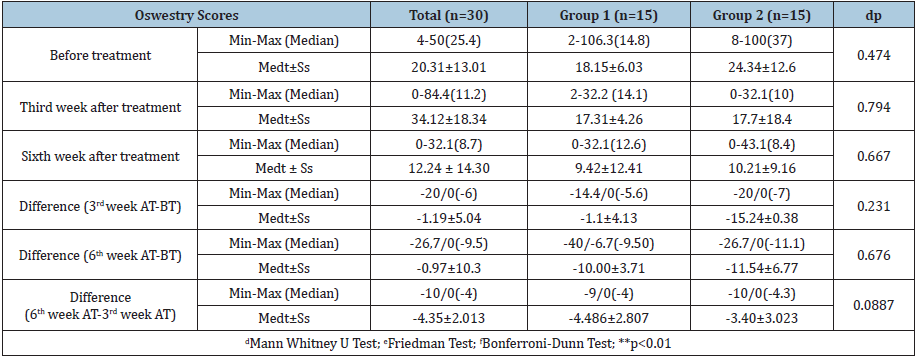
Characteristics of the sample
A total of 42 online learners entered the study and 36 (85.7%)
participants completed the entire protocol. The typical participant
was a 41 to 59 year old female, working in acute care with over
30 years nursing experience and employed part-time or casual
(Table 1). Less than half the participants (42.9%) indicated they
had post-graduate qualifications. The majority of participants
(88%) lived in one of the Eastern States of Australia and 69% were
born in Australia. Two respondents (4.8%) identified as being of
either Aboriginal or Torres Strait Islander descent. Participants’
experience in nursing/midwifery ranged from 2-50 years.
Table 1: Demographic characteristics of participants.
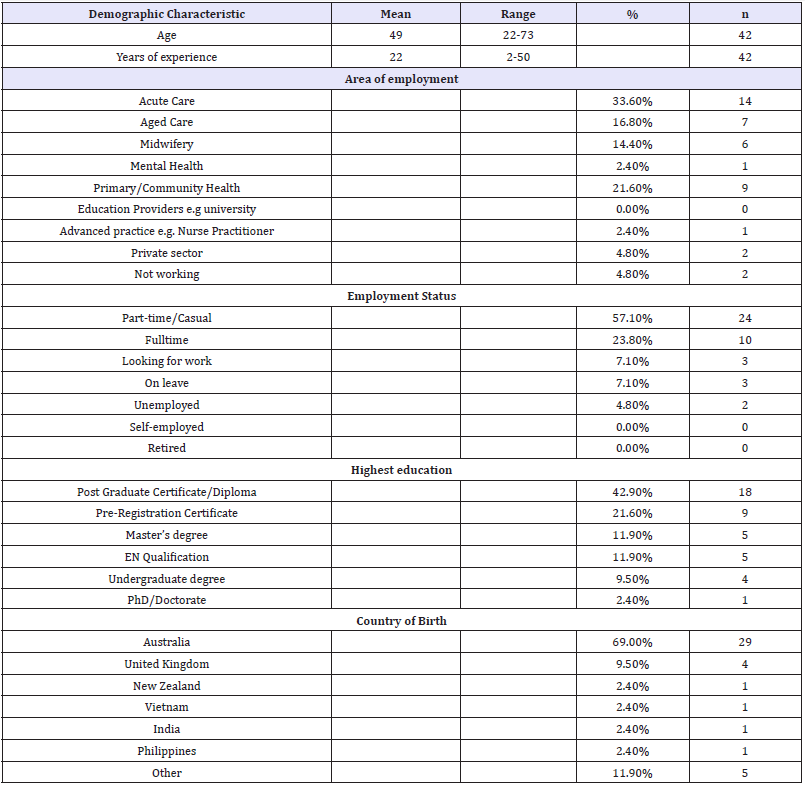
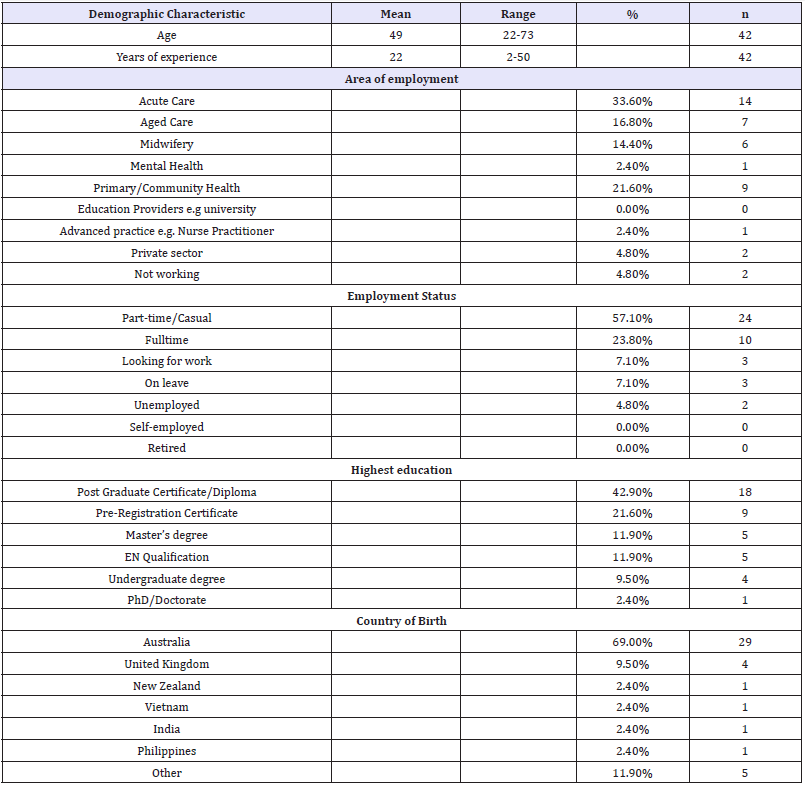
Motives for continuing professional education
The three most common reasons identified for undertaking
CPD were: maintaining nursing/midwifery registration (n=37;
88.1%), keeping up-to-date (n=34; 81%) and because they liked
learning (n=25; 59.5%) (Table 2). None of the participants chose
job promotion as a reason for undertaking CPD.
Table 2: Reasons for undertaking CPD (multiple options).
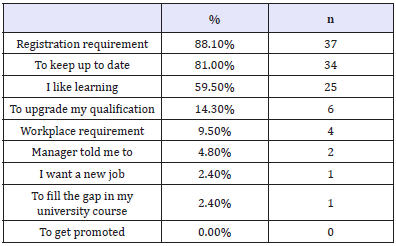
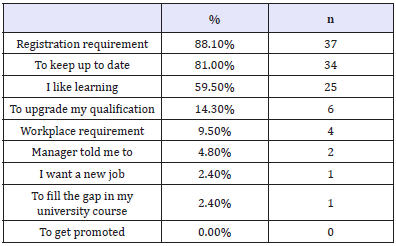
Continuing Professional Development via VLAs was mainly
preferred for its flexibility (n=38; 90.5%), 24 hour availability (n=34;
81%); and personalised pace of study (n=30; 71.4%). The currency
of the material delivered was rated 5th (n=19; 45.2%) in the nine
options provided (Table 3). Additional benefits of learning via VLAs
as stated by participants included: lack of education availability in
rural areas and being able to absorb more information.
Table 3: Advantages of Video Learning Activities (multiple options).
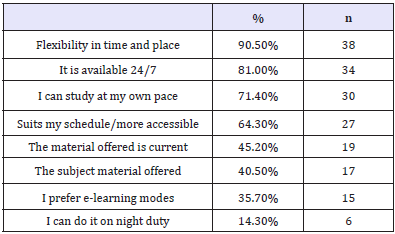
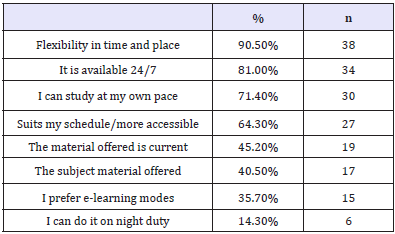
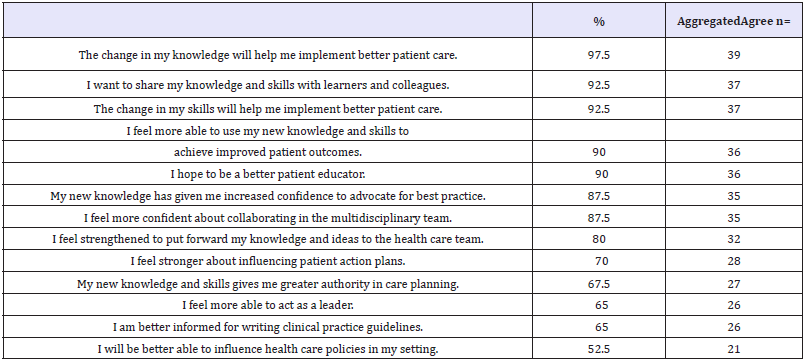
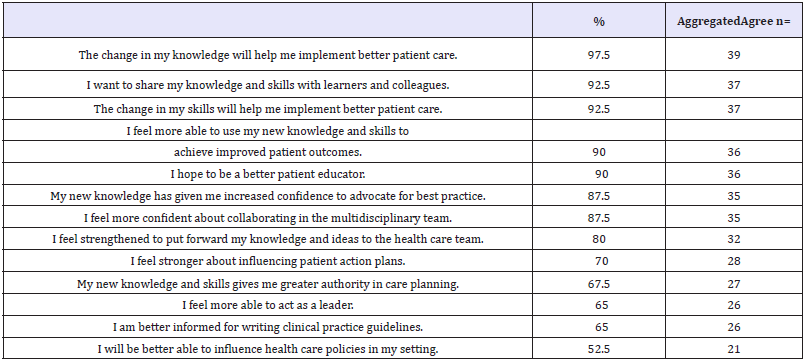
Influence of the chosen educational intervention
Forty (n=40; 95%) participants positively scored the impact
that their acquired knowledge from the VLAs chosen. Responses
were aggregated to reflect the majority’s responses in the
following categories: agree; neutral; disagree. Implementing better
patient care, sharing knowledge and skills and improving patient
outcomes had the strongest agreement about how new knowledge
had influenced participants (Table 4). Participants were unsure
they would be more able to influence healthcare (n=21; 52.5%),
implement a new or changed model of care (n=18; 45%); or present
a new or changed model of care at a conference (n=18; 45%).
Nearly half of the participants disagreed they hoped to publish a
new or changed model of care in a health journal (n=19; 47.5%).
Table 4: Influence from new knowledge.
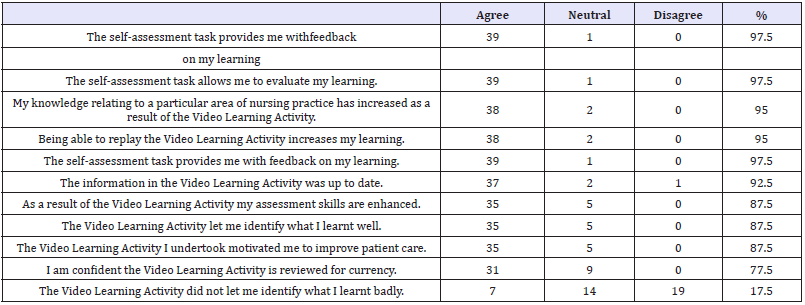
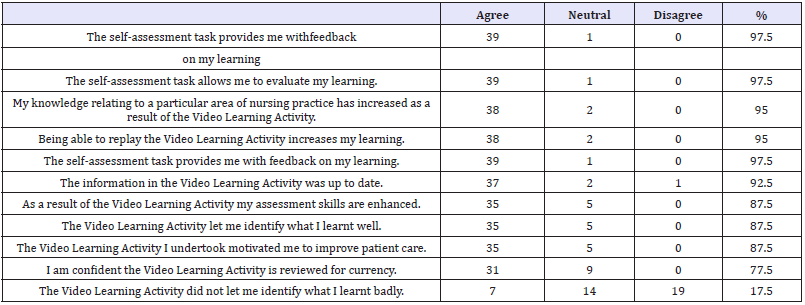
Augmented learning and self-assessment, increased knowledge
and enhanced nursing/midwifery skills were reportedly achieved
from the VLAs (87.5-97.5%) (Table 5). Most respondents found
the learning beneficial, motivational and empowering (87.5%) and
the VLAs allowed learners to identify what they had not learnt well
(47.5%).
Table 5: VLAs impact on Knowledge, attitudes and skills (n=40).
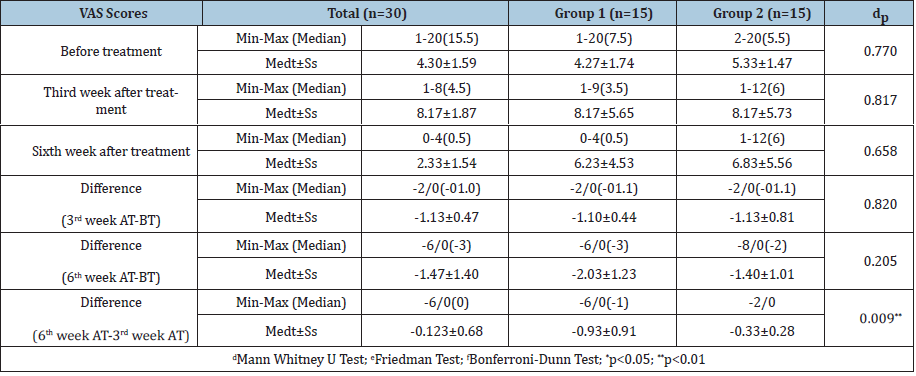
Effect of participating in the VLA/CPD
All respondents agreed/strongly agreed that participation
in the VLAs resulted in new knowledge/skills and that with new
knowledge they had increased confidence to advocate for best
practice. Thirteen (93%) reported that new knowledge and skills
enabled them to provide better patient care and 11 (78%) were
able to be a better patient educator. Others were able to contribute
to improved patient outcomes and contribute more strongly in the
health team (n=10; 71%). Reportedly, new knowledge and skills
contributed to a change in others’ and self-perception (n=8; 57%).
To be a leader and demonstrate influence were positively ranked
by 50% of respondents although 64.2% were unsure whether they
were better placed to gain a leadership position. In contrast to the
increase in clinical skills, scholarly activities such as publication and
presentation of new models of care were not considered achievable
(Table 6).
Discussion
The reported study evaluated users’ learning experience,
perceptions and outcomes from studying via online video learning
activities. Significantly, respondents found that participation in the
VLAs resulted in new knowledge/skills that resulted in improved
self-efficacy and enabled them to provide better patient care and be
a better patient educator. Consequently, this reportedly contributed
to improved patient health outcomes and stronger contribution
and influence in the multidisciplinary health team. The benefit
of continuing professional education in improving competence
has been identified [13]. Similar to findings from other studies of
participants’ perception of CPE, participants generally perceived
CPE as valuable and worthwhile and participated because it is
mandatory and helps them to retain their jobs [14].
Generally, participants were shown to be experienced, busy
professionals with a range of personal responsibilities. The majority
of respondents lived in three Australian states and none were
from overseas. Some respondents were born in countries other
than Australia and spoke a variety of languages including Spanish,
Mandarin, Hakka, Serbo-Croatian, Bosnian, Vietnamese, Tagalog
and Afrikaans. VLAs were mainly preferred for their flexibility,
availability; and personalised pace of studying. Participants were
self-directed with studying and self-identified their study needs.
Health professionals a positive attitude towards professional
development is recognised [13].
The reported demographics of the study population show the
aged care sector was the third most commonly reported area of
employment and acute care the first. As stated in the Australian
Institute of Health and Welfare (AIHW) report, in 2013, the work
setting of employed nurses and midwives with the highest full
time equivalent (FTE) rate was hospitals (excluding outpatients)
(Australian Institute of Health and Welfare, 2013).
The gender of the research participants reflects the gender
proportions of the nursing and midwifery workforce in Australia. In
2013, 10.4% of nurses and midwives working in Australia identified
as male (Australian Institute of Health and Welfare, 2013), a similar
proportion to those in the study (male 9.5%).
Participants in this study met the national Australian averages in
relation to age, experience, gender and working hours. Similar to the
respondents in this study (57.1%), data collected by the Australian
Health Practitioner Registration Authority (AHPRA) in 2013 also
shows that the majority of employed nurses and midwives (46.8%)
work part time [15]. The desire for fulltime employment did not
appear to be an incentive to study as the large majority (88.1%)
of respondents indicated CPD was a re-registration requirement
in Australia and consequently the primary reason for undertaking
CPD. Disappointingly, the need for further education for promotion
or other employment was not required, although this is not the
case in some professions where CPEs become a valued credential
that helps obtaining and keeping desirable positions, as well as
advancement to the next level in careers [16].
Congruent with data collected by AHPRA in 2013 which
shows that the majority of nurses were in the 50-54 year age
bracket, followed by 55-59 years, and 45-49 years, the majority
of respondents (61.4%) fell between the ages of 41 and 59 years
(Australian Institute of Health and Welfare, 2013). Ageing of the
nursing workforce has been cited as a reason for the workforce
shortages in nursing in Australia [15]. Accordingly, just under half
of the respondents (42.8%) reported significant nursing/midwifery
experience of over 30 years, ranging up to 50 years. Additionally,
high responsibility levels including work plus study plus carer
responsibilities may be a factor affecting nearly three quarters of
the participants who reported not working fulltime.
According to the Australian Bureau of Statistics, in mid-2011
there was 27% of the total population born outside of Australia
[1]. In accord, 31% of respondents were born outside Australia.
This population consisted of people who were born in UK, NZ,
Vietnam, India Philippines, Malaysia, El Salvador, Denmark, former
Yugoslavia and South-Africa, showing Australia’s multi-culturism
and therefore need to provide education that meets the needs of
nurses and midwives educated outside Australia.
The major benefits of online learning are known to include
convenience and increase accessibility to education. Respondents
reported that Video Learning Activities were mainly preferred over
classroom presentations for their flexibility, 24-hour availability,
and personalised pace of study. Preference due to the currency of
the material delivered was rated fifth of the nine options provided.
Additionally, respondents living in a rural area indicated there was
limited education available to them and the VLAs allowed nurses
and midwives working in rural and remote areas to undertake CPD
more readily and with greater flexibility. Geographic isolation and
poor technological and telecommunications infrastructure and
unemployment are identified as key barriers to CPE delivery and
access [13,14].
The majority of respondents reported they had online learning
experience with other education providers but rated the learning
impact of VLAs higher. Respondents reported that their previous
online learning experience had resulted significantly in a change
in their knowledge and skills, a change in their self-confidence and
change in their professional collaboration. This correlated with
the outcomes of the VLAs where all respondents agreed/strongly
agreed that participation in the VLA resulted in new knowledge/
skills and that with new knowledge they had increased confidence
to advocate for best practice. Examination of the influence of
interactive video on learning outcome and learner satisfaction in
e-learning environments has shown that students in the e-learning
environment that provided interactive video achieved significantly
better learning performance and a higher level of learner
satisfaction than those in other settings [5].
New knowledge and skills enables nurses to provide better
patient care and be able to be a better patient educator, to contribute
to improved patient outcomes and contribute more strongly in
the health care team. Interestingly respondents were unsure they
would be more able to influence healthcare, implement a new or
changed model of care or present a new or changed model of care
at a conference. Potentially, targeted education activities could
address this lack of confidence or knowledge.
VLAs were considered to be desirable and beneficial to
professional development. The majority of respondents did not
prefer classroom teaching over VLAs. Augmented learning and
self-assessment, increased knowledge and enhanced nursing skills
were reportedly achieved from the VLAs. Most respondents found
the learning useful and empowering (87.5%) and the VLAs allowed
learners to identify what they have not learnt well (47.5%).
Limitations
The response rate to the study in general was lower than
hoped and potentially limited the study and the sample size was
too small to allow for meaningful statistics. The response rate in
survey research is known to be problematical and a meaningful
reward for participation such as CPD points may have increased
participation. A larger sample with more diversity would have
benefited our results as may have the inclusion of learners studying
from international settings and experiencing different occurrences.
Nevertheless, all respondents completed the questionnaire in
enough detail for them to be analysed and contribute to answering
the research questions and the low response rate does not appear
to be impacted by non-response bias in a major way [17]. Due to the
small number of participants data is not representative of all nurses
and midwives.
For consistency and ability to compare and contrast data, using
the AIHW style of requesting specific information for principal
area of main job and work setting of main job reporting as basis
for asking area of employment would have been beneficial. The
majority of respondents lived in three of Australia’s eastern States
and unknowingly the survey did not allow for overseas postcodes
to be entered. A larger number of participants from rural areas of
Central Australia and Western Australia and overseas may have
provided different personal and professional demographics and a
different reflection of needs and perspectives.
Conclusion
This descriptive research study was conducted as an internal
service provision review and to determine the impact of CPD via online Video Learning Activities and the contribution made
to learners’ professional practice. The study has contributed to
the scarce literature about VLAs for CPD provided by private
enterprise and to closing the gap in what is known about e-service
usage for CPD by exploring learners’ experiences and learning
outcomes of VLAs via online learning. The findings suggest that it
may be important to integrate interactive instructional video into
e-learning systems.
Participants generally perceived CPE as valuable and
worthwhile and participated because it is mandatory and helps
them to retain their jobs. A second main finding from this study
is that nurses and midwives who undertook VLAs were confident
they had gained new knowledge and skills, which could be applied
to their practice. However, it is difficult to quantify or measure the
direct impact of this new knowledge and skills on actual practice.
This is because nurses and midwives may perceive they have applied
their new knowledge and skills but this may not have translated
into improved practice. Therefore, rather than only evaluate online
learning per se, it is important that education providers evaluate
the effectiveness in terms of knowledge transference to practice.
In addition, providers need to ensure the technology used and the
rigor of the education meets the needs of contemporary nurses and
midwives.
The project trialled a methodology that may be applied by other
education providers to assess the delivery of educational activities
that improve learners’ self-efficacy, knowledge and translation
of new knowledge and skills into practice. Challenges identified
included gaps in rural education that could be met by e-learning
and the need to continue to develop online learning opportunities.
Education providers need to continue to provide topics that address
the learning needs of nurses and midwives through a variety of
strategies. Mitchell [18] insists that the values and beliefs following
post registration education and practice decree that CPE must be
tailored to the needs of the individual and relevant to the practice
environment [18,19].
References
- Australian Bureau of Statistics (2013) Migration Australia, 2011-12
and 2012-13. Estimated resident population, Country of birth, State/
territory, Age and sex.
- Australian Institute of Health and Welfare (2013) Nursing and midwifery
workforce
- Gikandi JW, Morrow D, Davis NE (2011) Online formative assessment
in higher education: A review of the literature. Computers & Education
57(4): 2333-2351.
- Cobb SC (2004) Internet continuing education for health care
professionals: An integrative review. J Contin Educ Health Prof 24(3):
171-180.
- Zhang D, Zhou L, Briggs RO, Nunamaker JF (2006) Instructional video
in e-learning: Assessing the impact of interactive video on learning
effectiveness. Information & management 43(1): 15-27.
- He Y, Swenson S, Lents N (2012) Online Video Tutorials Increase
Learning of Difficult Concepts in an Undergraduate Analytical Chemistry
Course. Journal of Chemical Education 89(9): 1128-1132.
- Engelland BT, Hopkins C, Workman L, Singh M (1998) Service quality
and repeat usage: a case of rising expectations. Journal of Marketing
Management 8(2): 1-6.
- Stark CM, Graham Kiefer ML, Devine CM, Dollahite JS, Olson CM (2011)
Online Course Increases Nutrition Professionals’ Knowledge, Skills,
and Self-Efficacy in Using an Ecological Approach to Prevent Childhood
Obesity. J Nutr Educ Behav 43(5): 316-322.
- Ng KS, Abd R, Muhudin A (2014) E-Service Quality in Higher Education
and Frequency of Use of the Service. International Education Studies
7(3): 1-10.
- Martin BA, Bruskiewitz RH, Chewning BA (2010) Effect of a tobacco
cessation continuing professional education program on pharmacists’
confidence, skills, and practice-change behaviors. J Am Pharm Assoc
50(1): 9-16.
- Carlson J, OCass A (2010) Exploring the relationships between e-service
quality, satisfaction, attitudes and behaviours in content-driven e-service
web sites. The Journal of Services Marketing 24(2): 112-127.
- Pope C, Mays N, Popay J (2007) Synthesising Qualitative and Quantitative
Health Research: A Guide to Methods. Maidenhead: Open University
Press, UK.
- Keim KS, Gates GE, Johnson CA (2001) Dietetics professionals have
a positive perception of professional development.J Am Diet Assoc
101(7): 820-824.
- Curran VR, Fleet L, Kirby F (2006) Factors influencing rural health care
professionals’ access to continuing professional education. Aust J Rural
Health 14(2): 51-55.
- Graham EM, Duffield C (2010) An ageing nursing workforce. Aust Health
Rev 34(1): 44-48.
- Linney B J (1998) Why become a certified physician executive? Physician
exec 24(2): 50-52.
- Rok Seon Choung, G Richard Locke III, Cathy D Schleck, Jeanette Y
Ziegenfuss, Timothy J Beebe, Alan R Zinsmeister, et al. (2013) A low
response rate does not necessarily indicate non-response bias n
gastroenterology survey research: a population-based study. Journal of
Public Health 21(1): 87-95.
- Mitchell M (1997) The continuing professional education needs of
midwives. Nurse Educ Today 17(5): 394-402.
- Nsemo AD, John ME, Etifit RE, Mgbekem, MA, Oyira EJ (2013) Clinical
nurses’ perception of continuing professional education as a tool for
quality service delivery in public hospitals Calabar, Cross River State,
Nigeria. Nurse Educ Pract 13(4): 328-334.
For more articles in journal of nursing and healthcare impact factor