Intestinal Intussusception in an Adult Affected by Vanek Tumor: A Case Report by Morazán AD in Surgical Medicine Open Access Journal_journal of Surgical Medicine
Abstract
Inflammatory fibroid polyp (IFP) is a rare benign lesion, originating from the submucosa in the gastrointestinal tract. It generally appears as an isolated benign lesion, rarely located at the level of the ileum. Its origin is controversial. Clinical presentation varies depending on its location; invagination and obstruction are the most common indicative symptoms when the polyp is located at the level of the small intestine. We report the case of a 60-year old patient with abdominal pain, nausea and vomiting and a personal history of intermittent constipation. Radiological imaging objectified ileo-ileal invagination completely obstructing the ileum light. Segmental resection of the obstructed ileal segment and terminalterminal anastomosis were performed. The final diagnosis of IFP was established using histological examination.
Keywords: Inflammatory fibroid polyp; Ileum; Invagination
Introduction
Adult intussusception is relatively rare, constituting only 1% of patients with bowel obstructions. Adult intussusception is mostly caused by tumors and 80% of the tumors associated with small bowel intussusception are benign. Vanek tumor (inflammatory fibroid polyp) is a rare pseudo-tumorous lesion of the gastrointestinal tract first described by Vanek in 1949 [1]. It occurs most frequently in the gastric antrum of adults, inflammatory fibroid polyp (IFP) rarely cause ileal intussusception [2]. The IFP is a benign lesion that arises from the submucosa of the gastrointestinal (GI) tract, most commonly in the antrum (70%) and ileum (20%) and, only occasionally, in the duodenum and jejunum. Its frequency from 1% to 4% of diagnoses among benign lesions, and usually occurs between the fifth and the seventh decade of life [3]. The underlying cause of IFPs is still unknown. Many have suggested etiologies possibly related to chemical, physical, or metabolic triggers. Genetic study of IFP showed mutations in platelet derived growth factor alpha (PDGFRA) in some cases. The frequency of mutations among case series ranges from 21.7% to 69.6%. Activating PDGFRA mutations occur in exons 12, 14 and 18. It also shows for the presence of androgen receptor-positive cells whose location corresponds with the distribution of Ki67- positive cells. When localized in the small bowel, the presenting symptoms are colicky abdominal pain and obstruction. Intussusception due to IFPs is uncommon; moreover, jejunojejunal and ileoileal intussusception has only rarely been reported [4-14]. We present the case of a 60-year-old male presenting with symptoms preceding an intestinal obstruction caused by an ileoileal intussusception with an inflammatory fibroid polyp acting as the lead point.
Clinical Case
A 60-year-old male patient, married, farmer, from Tegucigalpa, with a history of a month and a half of evolution, insidiously presenting moderately intense abdominal cramps, diffuse location with predominance in the right iliac fossa and mesogastrium, short duration, accompanied by nausea, vomiting twice a week, which is attenuated after the intake of analgesics and antispasmodics. Evaluated by general practitioner and managed with antispasmodics, changes in lifestyle and diet. The patient continued with insidious, sporadic, and self-limited episodes of pain until one day prior to admission presented an exacerbation with increased intensity without attenuating the intake of analgesics and antispasmodics, so he went to the emergency surgery assessment general. Pathological personal history of systemic arterial hypertension managed with irbersartan 300mg orally every day, benign prostatic hyperplasia treated with alfuzosin once daily, grade I obesity. On physical examination, the patient presented complaining with pain facies, hemodynamically stable with vital signs of BP 130/90mmhg, FC 96x, FR 16x, temperature of 36.5 ℃ without data of respiratory distress, oxygen saturation of 98% with ambient air , chest with well-ventilated lung fields with vesicular murmur, globular abdomen at the expense of adipose tissue, hypoactive intestinal noises 2 per minute, without distension, percussion without alterations, soft, depressible, moderate pain on deep palpation in the iliac fossa and right flank, no involuntary muscular resistance, no data of peritoneal irritation, no palpable tumors or visceromegalies. Genitals and inguinal region without alterations. No stool to the rectal touch. Laboratory tests were requested with the following results: Hb 12.1g/dL, H to 38.5mL/dL, VCM 91.9μm3, WBC. 10,800/mm3, neutrophils 72.2%, platelets 474,000/mm3; Biochemical: Glucose 100mg/dL, Na 140mEq/L, K 4.4mEq/L, creatinine 1.0mg/dL, BUN 13.8mg/dL, urea 32.5mg/dL, Alb 5.1g/dL, TGO 23U/L, TGP 36U/L.
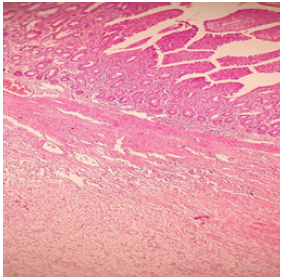
Subsequently, his study was complemented by requesting abdominal tomography. In which a proximal ileal loop was observed with the presence of distal cystic tumor that measures approximately 3.5cm with proximal dilation of this intestinal loop with a hydro-air level, related to intestinal invagination. No data of intestinal obstruction, free fluid, or pneumoperitoneum were observed (Figure 1). He was admitted for surgical treatment with a diagnosis of intestinal invagination. A diagnostic laparoscopy was performed and turned in open laparotomy with the following findings, a firm consistency tumor in the small intestine at the level of the ileum 7cm long and 3.5cm in diameter, occupying the entire lumen of the intestine, with an ileo-ileal invagination segment of approximately 15cm (Figure 2). The tumor was evaluated small intestine segment which measures 7cm long by 3.5cm in diameter with a light brown, smooth, shiny serosa, wall 4cm thick, trabeculated mucosa preserved in the intestinal wall, a nodular mass measuring 4 by 3.5cm, gray, cream attached directly to the wall, clean surgical edges of soft consistency and gelatinous appearance, well defined, not encapsulated with moderate amount of non-foul, non-hot inflammatory fluid (Figure 3). It was decided to perform resection and ileo-ileum anastomosis, the patient evolved satisfactorily and began diet 24 hours post-operative and discharged 4 days later without complications. Histological reported myxoid-like lesion made up of elongated fibroblasts, also with an inflammatory infiltrate polyp accompanied by eosinophils. It grows in the submucosa, pushes and ulcerates the submucosa, with an acute inflammatory reaction. well-defined tumor without cell atypia or mitosis, normal surgical edges (Figure 4).
Figure 1: Proximal ileal loop with the presence of distal cystic tumor that measures approximately 3.5cm with proximal dilation of this intestinal loop with a hydro-air level, related to intestinal invagination.
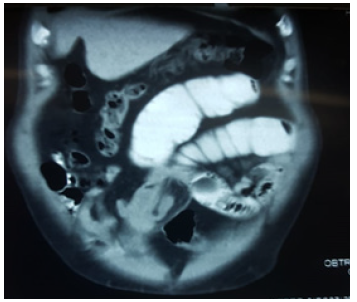
Figure 2: Firm consistency tumor in the ileum 7cm long and 3.5cm in diameter, occupying the entire lumen of the intestine, with an ileo-ileal invagination.

Figure 3: The tumor with a light brown, smooth, shiny serosa, trabeculated mucosa preserved in the intestinal wall, a nodular mass, cream attached directly to the wall, clean surgical edges of soft consistency and gelatinous appearance, well defined, not encapsulated.
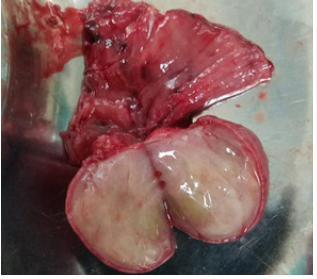
Figure 4: Histological reported myxoid-like lesion made up of elongated fibroblasts, also with an inflammatory infiltrate polyp accompanied by eosinophils.
References
- Daum O, Hes O, Vanecek T, Benes Z, Sima R, et al. (2005) Vanek’s Tumor (Inflammatory Fibroid Polyp). Report of 18 cases and comparison with three cases of original Vanek’s series. Annals of Diagnostic Pathology 7(6): 337-347.
- Akbulut S, Mahsuni M, Cakabay Bahri, Sule Bakir, Ayhan Senol (2009) Giant inflammatory fibroid polyp of ileum causing intussusception: a case report. Cases J 2: 8616.
- Fazzio C, Madeira E (2015) Inflammatory fibroid polyp (Vanek’s polyp): a case report and literature review. J Bras Patol Med Lab 51(2): 117-120.
- Bays D, Anagnostopoulos G, Katsaounos E, Filis P, Missas (2004) Inflammatory fibroid polyp of the small intestine causing intussusception: A report of two cases. Dig Dis Sci 49(10): 1677-1680.
- Jukic Z, Ferencic Z, Radulovic P, Mijic A (2014) Estrogen and androgen receptors in inflammatory fibroid polyp (Vanek’s Tumor): Case report. Anticancer Res 34(12): 7203-7206.
- Lee C, Yuen MK (2014) Inflammatory fibroid polyps causing intussusception in adult patients: Two case reports and review of literature focusing on radiological features. Hong Kong J Radiol 17: 271-276.
- Rossi P, Montuori M, Balassone V, Ricciardi E, Anemona L, et al. (2012) Inflammatory fibroid polyp. A case report and review of the literature. Ann Ital Chir 83(4): 347-351.
- Ahtil R, Bensghir M, Meziane M, Houba A, Jaafari A, et al. (2017) Rare etiology of subocclusive syndrome: inflammatory fibroid polyp of the ileum, about a clinical case. Pan Afr Med J 26: 146.
- Madriz DeHaan P, Martínez Y, Gutiérrez F (2014) Intestinal intussusception due to an inflammatory fibroid polyp (Vanek's tumor). Legal Medicine of Costa Rica-Virtual Edition 31(1): 1409-1415.
- Paikos D, Moschos J, Tzilves D, Koulaouzidis A, Kouklakis G, et al. (2007) Inflammatory fibroid polyp or Vanek’s tumour. Dig Surg 24: 231-233.
- Yakan S, Calıskan C, Makay O, Denecli AG, Korkut MA (2009) Intussusception in adults: Clinical characteristics, diagnosis and operative strategies. World J Gastroenterol 15(16): 1985-1989.
- Gara N, Falzarano J, Limm W, Namiki T (2009) Ileal inflammatory fibroid polyp causing chronic ileocolic intussusception and mimicking cecal carcinoma. World J Gastrointest Oncol 1(1): 89-92.
- Bassam Abboud (2015) Vanek’s tumor of the small bowel in adults. World J Gastroenterol 21(16): 4802-4808.
- Zakaria A, Daradkeh S (2012) Jejunojejunal intussusception induced by a gastrointestinal stromal tumor. Case Rep Surg 2012: 173-680.




I am really impressed the way you have written the blog. Hope we are eagerly waiting for such post from your side.
ReplyDeleteMaster the Melodic Language: Learn German Language Today
Discover the Beauty and Diversity of the Arabic Language