A Clinical Challenge: A Rare Case of Neoadjuvant Chemotherapy for Stage IB3 Cervical Cancer in Pregnancy by Lei Huang in Advancements in Case Studies_online case studies
Abstract
Treatment of cervical cancer during pregnancy (CCP) is controversial and individual. Here, we present a successful case of a 31-year-old woman who was diagnosed of stage IB3 cervical squamous cell carcinoma at her 14th week of pregnancy. As the patient had a strong desire to preserve her pregnancy, she was first treated with 4 cycles of neoadjuvant chemotherapy (NACT), cisplatin 75mg/m2 and paclitaxel 175mg/m2 per 21 days. Then a cesarean section followed by a radical hysterectomy and pelvic lymphadenectomy was performed at her 36 weeks and 3 days of gestation, and no post operational adjuvant therapy was performed. With a follow-up for 12 months post operation, the neonate and the mother showed no complications related to the treatments and there was no recurrence of the patient during follow-up.
Keywords: Neoadjuvant chemotherapy, Cervical cancer, Pregnancy
Abbreviations: CC: Cervical Cancer; CCP: Cervical Cancer during Pregnancy; NACT: Neoadjuvant Chemotherapy; SCC: Squamous Cell Carcinoma
Introduction
Cervical cancer (CC) is the most common gynecological malignancy diagnosed in pregnancy with a crude incidence rate of 1.4-4.6 per 100,000 pregnancies [1,2]. In China, the incidence of cervical cancer during pregnancy was estimated 4 per 100000 pregnancies [3]. With the popularization of cervical cancer screening for the past few years, most cervical cancers were diagnosed in the early stage. It was reported that more than two thirds of cervical cancer combined with pregnancy were diagnosed at stage I, and 93.5% of the patients had a first or second term pregnancy [4]. The options of therapy for cervical cancer during pregnancy are diversity and individual. It depends on the gestation weeks, patients’ desire, stage of cancer, lymph node involvement and so on. At present, whether pregnancy will accelerate the progression of cervical cancer is debatable, and the long-term prognosis for different therapies is still unknown to us. Therefore, more evidence-based medical experiences are needed to guide the treatments for CCP. In this article, we presented a successful case of a 14th week pregnancy woman diagnosed with stage IB3 cervical squamous cell carcinoma.
Case Presentation
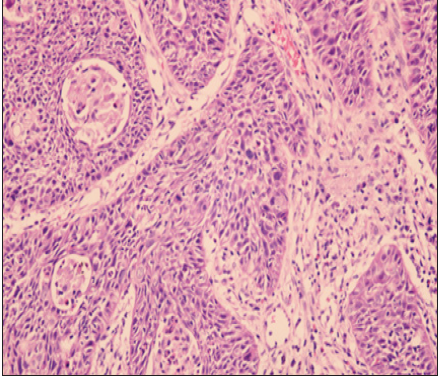
A 31-year-old woman-gravida 2, para 1-who was at her 14th weeks of gestation, presented for, a 2-month history of unexpected vaginal bleeding and 2-year history of vaginal bleeding after intercourse. She had never had a previous cervical cytological examination and HPV screening before. Gynecologic pelvic examination revealed an approximately 4.5cm in diameter cervical lesion that encompassed the entire cervix with contact hemorrhage. The cervical lesion was limited to the cervix and without involving the bilateral parametrium and vagina. A cervical biopsy was performed and the pathology results showed an invasive, moderately differentiated, squamous cell carcinoma (SCC). The pathological result is shown in Figure 1. MRI of the abdomen and pelvis confirmed a cervical lesion of 4.2×3.4cm in diameter, without extended to parametrium and lymph nodes. As the patients had a strongly desired to continue the pregnancy, we organized a multidisciplinary consultation including gynecologic oncology, maternal-fetal medicine and neonatology, and finally made an individualized treatment plan for her. The patient was extensively informed of her diagnosis, the risks for continuing pregnancy and the benefits for terminating pregnancy. 4 cycles of neoadjuvant chemotherapy with cisplatin 75mg/m2 and paclitaxel 175mg/m2 every 3 weeks was administered.
Figure 1: Biopsy of cervical mass showing invasive squamous cell carcinoma.
After the first cycle of chemotherapy, the cervical tumor appeared to decrease in size by physical exam. Surprisingly, no tumor was found by physical examination and imaging examination after 4 cycles of chemotherapy was finished. The patient received antenatal care conventionally, and the fetal showed no abnormalities during pregnancy. At 36 weeks and 3days’ gestation, a cesarean section followed by radical hysterectomy and pelvic lymphadenectomy was performed. The infant was delivered with an Apgar scores of 9 and 10 at 1 and 5 minutes respectively, and weighing 3130g. Intraoperative exploration, found no lesions on the bladder, rectum, liver, and diaphragm. The postoperative pathological results showed a moderately differentiated cervical carcinoma with diameters of 0.3cm at the position of 3 and 10 o’clock of cervix, the depth of lesion that invaded into cervical muscle layer was 0.3cm, and an individual cancer lesion about 0.6x0.3cm was found at the position of 4 o’clock of cervix, without lymph vascular space invasion. No further adjuvant therapy was performed. Physical examination, SCCA screening and pelvic ultrasound were performed every 3 months during her follow-up. It has been one year since the operation; no sign of recurrence was found for the patient. Moreover, the infant was also given a routine child health care and no abnormality was discovered.
Discussion
It was reported that cancer occurred in 0.05 to 0.1% of all
pregnancies, the most common gynecologic cancer presenting
during pregnancy is cervical cancer [5]. CCP was usually to be
ignored and misdiagnosed for confusing with abortion or placenta
previa. In many hospitals of China, cervical cancer screening
during the first trimesters of pregnancy or pre-pregnancy was
not taken seriously, and HPV vaccine was not so widely used at
present, Therefore, the incidence of CCP in China is relative higher
than in developed countries. As depicted above, treatment for
cervical cancer is intractable and individual. For the first or early
second trimester of pregnancy, 44% of gynecologist preferred to
choose termination of pregnancy and 77% considered a delay and
later treatment if the patient had a strong desire to preserve the
pregnancy [6]. Solid data on how pregnancy affects the outcome
of gynecological cancers is missing, although a few reports have
shown that CCP might not be associated with a poorer prognosis
[7,8]. However, the proposed treatment for CCP should adhere to
the standard treatment for non-pregnant patient. According to the
guidelines of European Society for Medical Oncology (ESMO), in
stage IB3 of CCP, NACT as the only pregnancy-preserving option
that be recommended, although further studies are still needed.
Follow-up without therapy in such cases was likely to compromise
the prognosis and was not recommended. The role of staging
lymphadenectomy was controversial [9]. In this case, NACT for CCP
in stage IB3 had obtained satisfactory effect and also reduced the
difficulty of operation. Studies showed that use of chemotherapy
in the second and third trimester of pregnancy did not increase
the risk of fetal malformations, but might be associated with
IUGR, prematurity, lower birth weight and higher rate of stillbirth
[10,11]. There was also no significant difference in overall survival
and progression‐free survival between pregnant women receiving
cisplatin combined with other chemotherapeutic drugs and those
receiving cisplatin alone [12].
However, there are no guidelines existed regarding to
chemotherapeutic dosages during pregnancy, and we currently use
the same chemotherapeutic dosages for non-pregnant and pregnant
patients. Moreover, chemotherapy should not be administered
after 35 weeks since unpredictable labor will be occurred at
any time [13]. As for CCP diagnosed in stage IIB or higher, it was recommended for termination of pregnancy, while a few studies
reported successful preservation of pregnancy and good prognosis.
Innocenza Palaia reported a case of a woman was diagnosed with
cervical cancer in stage IIB at 19th weeks gestation, she was given
an NACT for 3 cycles and then underwent a cesarean section
followed by a radical hysterectomy and pelvic lymphadenectomy as
well. Because of her severe allergic reaction for paclitaxel, she was
treated with cisplatin alone. The outcomes of the patient and infant
were also favorable during follow-up [14]. Ying Guo reported a case
of successful maintained pregnancy for stage IB3 cervical cancer
diagnosed at 13 weeks, the patient received 5 courses of systemic
chemotherapy with carboplatin and paclitaxel every 3 weeks,
followed by caesarean section and radical hysterectomy. Both the
mother and infant are in good general condition [15].
Conclusion
In conclusion, cervical cancer during pregnancy represents a tough challenge because of its impact on fetal development, unknown oncologic outcomes and diversity management. If one CCP patient have a strong desire to preserve pregnancy, NACT combined operation was considered to be a common and effective method to treat CCP in early or mid-stages. Of course, more evidence of evidence-based medicine and long-term follow-up are needed to testify the safety and effects of the treatments.
References
- Perrone AM, Bovicelli A, Andrilli DG, Borghese G, Giordano A, et al. (2019) Cervical cancer in pregnancy: Analysis of the literature and innovative approaches. J Cell Physiol 234(9): 14975-14990.
- Kyrgiou M, Horwell DH, Farthing A (2015) Laparoscopic radical abdominal trachelectomy for the management of stage IB1 cervical cancer at 14 weeks gestation: Case report and review of the literature. BJOG 122(8): 1138-1143.
- Beharee N, Shi Z, Wu D, Wang J (2019) Diagnosis and treatment of cervical cancer in pregnant women. Cancer Med 8(12): 5425-5430.
- Charkviani L, Charkviani T, Natenadze N, Tsitsishvili Z (2003) Cervical carcinoma and pregnancy. Clin Exp Obstet Gynecol 30(1): 19-22.
- Cordeiro CN, Gemignani ML (2017) Gynecologic malignancies in pregnancy: Balancing fetal risks with oncologic safety. Obstet Gynecol Surv 72(3): 184-193.
- Han SN, Kesic VI, Van Calsteren K, Petkovic S, Amant F (2013) Cancer in pregnancy: A survey of current clinical practice. Eur J Obstet Gynecol Reprod Biol 167(1): 18-23.
- Van Tienen TG, Stensheim H, Sophie DF, Bjørn M (2009) Cause-specific survival for women diagnosed with cancer during pregnancy or lactation: A registry-based cohort study. J Clin Oncol 27(1): 45-51.
- Halaska MJ, Uzan C, Han SN, Fruscio R, Dahl Steffensen K, et al. (2019) Characteristics of patients with cervical cancer during pregnancy: A multicenter matched cohort study. An initiative from the international network on cancer, infertility and pregnancy. Int J Gynecol Cancer.
- Amant F, Berveiller P, Boere IA, Cardonick E, Fruscio R, et al. (2019) Gynecologic cancers in pregnancy: Guidelines based on a third international consensus meeting. Ann Oncol 30(10): 1601-1612.
- Ngu SF, Ngan HY (2016) Chemotherapy in pregnancy. Best Pract Res Clin Obstet Gynaecol 33: 86-101.
- Amant F, Vandenbroucke T, Verheecke M, Fumagalli M, Halaska MJ, et al. (2015) Pediatric outcome after maternal cancer diagnosed during pregnancy. N Engl J Med 373(19): 1824-1834.
- Song Y, Liu Y, Lin M, Sheng B, Zhu X (2019) Efficacy of neoadjuvant platinum-based chemotherapy during the second and third trimester of pregnancy in women with cervical cancer: An updated systematic review and meta-analysis. Drug Des Devel Ther 13: 79-102.
- Gungorduk K, Sahbaz A, Ozdemir A, Gokcu M, Sanc M, et al. (2016) Management of cervical cancer during pregnancy. J Obstet Gynaecol 36(3): 366-371.
- Palaia I, Pernice M, Graziano M, Bellati F, Panici PB (2007) Neoadjuvant chemotherapy plus radical surgery in locally advanced cervical cancer during pregnancy: A case report. Am J Obstet Gynecol 197(4): e5-e6.
- GuoY, Zhang D, Li Y, Wang Y (2020) A case of successful maintained pregnancy after neoadjuvant chemotherapy plus radical surgery for stage IB3 cervical cancer diagnosed at 13 weeks. BMC Pregnancy Childbirth 20(1): 202.




No comments:
Post a Comment