Fluro Imaging: A Boon to Difficult Subarachnoid Block by Anisha Nagaria in Developments in Anaesthetics & Pain Management_Developments in Anaesthetics & Pain Management
Abstract
26-year young female, a known case of long-standing ankylosing spondylitis and suspected case of osteopetrosis having fracture shaft femur had presented to us for lower limb surgery. Difficult spine and limited neck movement due to fusion of vertebras make regional and general anesthesia a challenge for anesthesiologist. After failure of traditional approach to central neuraxial block, fluoroscopic guided block spinal anesthesia was achieved successfully. But with experienced hands, Fluro imaging helps to deal with difficult situation like ankylosing spondylitis safely..
Keywords: Ankylosing spondylitis; Difficult spine; Fluro imaging
Abbreviation: AS: Ankylosing Spondylitis; LS: Lumbosacral; AP: Anteroposterior; SAB: Subarachnoid Block; USG: Ultrasonography; OT: Operation Theater
Introduction
Ankylosing spondylitis (AS) is a chronic inflammatory disease of unknown etiology, having classic “bamboo spine” appearance due to formation of bony bridges between vertebrae. That makes administration of both general and regional anesthesia difficult. Hard lumbosacral (LS) spine with narrow intervertebral spaces, difficult positioning for intubation and spinal anesthesia, and sever pain at the fracture site poses challenge to anesthesiologist. Use of C-arm guided identification of the spine helps in finding severity of LS involvement and identifying widest open intervertebral space is of interest in case of difficult spinal anesthesia. This article reports a successful conduct of orthopedic case, having very difficult spine under C-arm guided subarachnoid block, following failed landmark technique.
Case Report
A 26-year female, a known case of AS, presented with right sided fracture femur after a minor trauma was posted for plating. Patient also had multiple impending fractures in upper and lower limb. At the time of admission, patient was severely anemic (Hb-4.5gm/ dl) which was corrected with multiple blood transfusion (Hb- 9.63gm/dl). MRI of Lumbosacral (LS) spine showed significantly hypertrophied facet joints along with possibility of myelofibrosis/ myeloproliferative disease. These findings suggested possibility of osteopetrosis also, but no other anomalies were found in thorough Pre-anesthesia evaluation. Patient had minimal neck extension and modified mallampati grade 2. After written informed consent patient was electively posted for surgery.
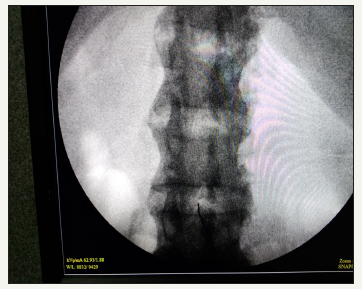
In Operation theater (OT), multipara monitors were attached. A wide bore i.e. line was secured and RL infusion was started. Difficult airway cart was kept ready. Patient was made to sit and under all aseptic precaution, Lumbar punctures were attempted at different spinal levels by median or paramedian approach through landmark technique, but it failed even after multiple attempts. So, it was decided to attempt fluoroscopic guided subarachnoid block under c-arm in same sitting position. An anteroposterior (AP) image of the lumbosacral spine Figure 1&2 showing minimal assessable window at L3-L4 intervertebral space (Figure 3) by variable degrees of lateral and oblique C-arm rotation was obtained. Subarachnoid space was approached in single prick with 25-gauge quincke-Babcock spinal needle using end on view between L3-L4 space. After confirming free flow of CSF, 0.5% Bupivacaine heavy 3.5ml was injected. Patient was immediately made to lie-down in supine position and a level of T10 was achieved. Throughout the surgery hemodynamic vitals were maintained. Surgery was completed uneventfully.
Discussion
Ankylosing spondylitis (AS) is a chronic inflammatory disease of the axial skeleton and peripheral joints, characterized by fusion of adjacent vertebrae, which leads to loss of flexibility of the back and neck. [1] These changes make AS a case of difficult airway and difficult central neuraxial blockade. Cervical spine involvement, with limited movements, makes tracheal intubation difficult which becomes a challenge for anesthesiologist [2]. Prior planning, use of all difficult airway measures and expert hands will ease the situation. Hyperextension of neck should be avoided to prevent cervical fracture. Fiberoptic bronchoscopy can be used successfully to secure the airway [3]. Establishing regional anesthesia in ankylosed spine is also challenging due to reduced articular mobility, obliteration of the inter-spinal spaces and impossibility to position the patient adequately [4].
Figure 1:Position of C-arm and patient in sitting position for AP view of LS spine.

Figure 2:position of c-arm and patient for AP view of LS spine.

Figure 3:AP view from image intensifier showing fused vertebrae and end on view of spinal needle from minimal assessable space between L3-L4 vertebra through which subarachnoid block was approached.
We suspected osteopetrosis also in our patient, because of presence of multiple impending fracture and MRI finding of myelofibrosis, which was another challenge for us, as these patients, add to difficulty in position due to brittle bones. The anaesthetic options are limited and technically difficult with both airway and spine involved in the disease process. The osteoporotic bones are difficult to drill, and surgical time can escalate [5].
Landmark guided subarachnoid block (SAB) becomes difficult and sometime impossible in cases of AS. So, different techniques were reported in various articles for approaching subarachnoid block in AS. The paramedian approach was mentioned in various case reports, this avoids the ossified midline ligaments (interspinous ligament and ligamentum flavum) and has a lower risk of encountering the exiting spinal nerve root [6]. KH Leung et al. [6] had reported a case of sever AS where successful elective mini laminectomy was performed under local anesthesia to approach Subarachnoid space. They had also mentioned about possible complications like inadvertent injury of neural tissues during laminotomy, fracture of the spine and risk of a high spinal anesthetic block with cardio-respiratory impairment. Ultrasonography (USG) of the lumbar spine may facilitate successful central neuraxial blockade in such patients, by indicating the presence and location of a soft tissue window into the vertebral canal [7,8]. Rakesh Goyal and colleagues have presented a case of bilateral THR, who was previously operated under general anesthesia due difficult spine. Later in his next surgery electively planned USG guided SAB was achieved successfully [9].
Neuraxial anesthesia is technically difficult in patients with AS but fluoroscopic guided imaging could successfully be performed. It has proved to be useful alternative option in difficult spinal anesthesia but requires expertise and associated with biological hazards to the patient and staff present in the OT. Reducing the exposure time, distance from radiation source, proper shielding, use of low dose and pulse mode helps in reducing radiation exposure while fluoroscopic guided approach to SAB [6]. SM Channabasappa and his colleagues have reported a case of fluoroscopic guided SAB in patient posted for uretroscopic removal of stone. Fluoroscopic guided transforaminal approach to epidural space was attempted in prone position after failed classical approach [2].
In most of the articles, fluoroscopic guided SAB was performed in prone and in lateral position. We had preferred sitting position for patient as our patient had multiple fracture and putting her in lateral or prone position would had been painful and to reposition patient in supine position would become difficult and time taking. This could have led to inadequate level of anesthesia because we used hyperbaric drug. In the sitting position c-arm was placed in anteroposterior (AP) direction and SAB was achieved.
Conclusion
Ankylosing spondylitis although is a challenge for anesthetist for both managing airway and regional anesthesia but should not be considered unachievable in any case. Understanding the situation and proper planning could be key to success. Fluoroscopic guided neuraxial block is a big boon to difficult spinal anesthesia in expert hand and can be preferred as choice in anticipated difficult spine.
References
- Woodward LJ, PCA Kam (2009) Ankylosing spondylitis: Recent developments and anesthetic implications. Journal of Association of Anesthesia of Great Britain and Ireland 64(5): 540-548.
- Channabasappa SM, Dharmappa S, Pandurangi R (2016) Fluoroscopy guided transforaminal epidural anesthesia in ankylosing spondylitis. Saudi J Anaesth 10(1): 101-103.
- Dave N, Sharma RK (2004) Temporomandibular joint ankylosis in a case of ankylosing spondylitis anaesthetic management. Indian J Anaesth 48: 54-56.
- Preeti R, Geeta AP, Bharati AT (2016) Management of a case of ankylosing spondylitis for percutaneous nephrolithotomy in prone position under combined spinal epidural anesthesia. Medical Journal of 9(6): 765-767.
- Ashima S, Poojitha R, Sreedhar R, Ramchandran G (2015) Marble bone disease and the anesthesiologist. Indian Journal of Anesthesia 59(6): 390-391.
- Leung KH, Chiu KY, Wong YW, Lawmin JC (2010) Case report: Spinal anesthesia by mini-laminotomy for a patient with ankylosing spondylitis who was difficult to anesthetize. Clin Orthop Relat Res 468(12): 3415- 3418.
- Chin KJ, Macfarlane AJ, Chan V, Brull R (2009) A case report: The use of ultrasound to facilitate spinal anesthesia in a patient with previous lumbar laminectomy and fusion. J Clin Ultrasound 37(8): 482-485.
- Chin KJ, Vincent C (2010) Ultrasonography as a preoperative assessment tool: Predicting the feasibility of central neuraxial blockade. Anesthesia & Analgesia 110(1): 252-253.
- Goyal R, Singh S, Shukla RN, Singhal A (2013) Management of a case of ankylosing spondylitis for total hip replacement surgery with the use of ultrasound-assisted central neuraxial blockade. Indian J Anaesth 57(1): 69-71.
https://crimsonpublishers.com/dapm/fulltext/DAPM.000524.php




No comments:
Post a Comment