Same Story with Different Endings in HER2- Positive Breast Cancer: Why the Benefit of Pertuzumab is Robust in the Metastatic Scenario and Modest in the Adjuvant Setting? by Jayesh Sagar* in Surgical Medicine Open Access Journal_ Journal of Surgical Medicine
Abstract
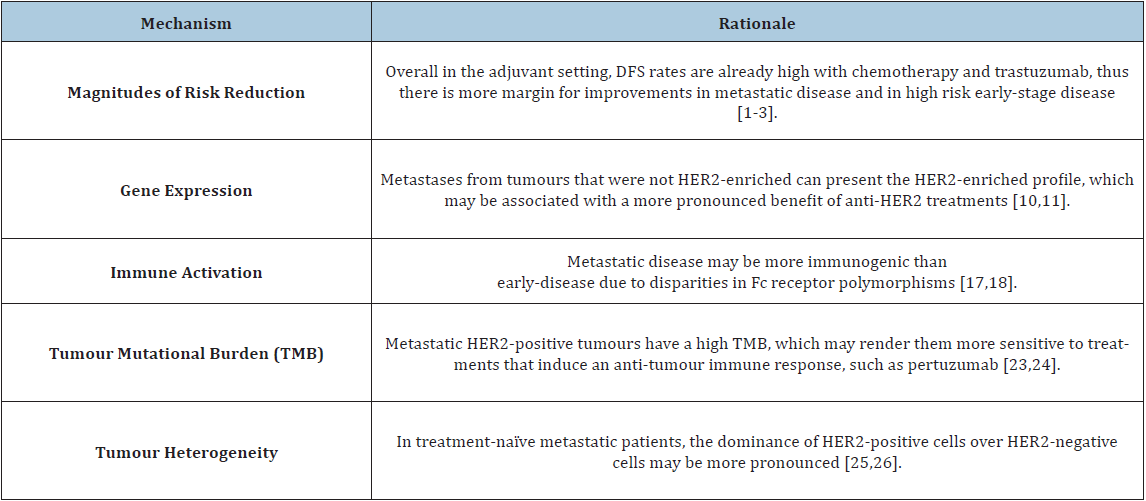
The
addition of pertuzumab to chemotherapy and trastuzumab yielded an impressive
improvement in the outcomes of metastatic HER2-positive breast cancer patients
[1]. Intriguingly, the same magnitude of benefit could not be reproduced with
pertuzumab in the adjuvant setting, being the reasons for this discrepancy
unknown [2,3]. In this manuscript, we discuss clinical and biological
differences between metastatic and early-stage HER2-positive breast cancer, and
conclude by proposing potential explanations for the distinct magnitudes of
benefit of pertuzumab in different disease settings.
Magnitude of Risk Reduction
When
evaluating a new treatment in the context of a clinical trial, events occurring
in experimental and control arms are compared [4]. Early-stage HER2-positive
breast cancer patients treated with adjuvant chemotherapy and trastuzumab
had a 87.8% recurrencefree survival rate at 6 years as per the recently updated
results of the APHINITY trial [3]. In the metastatic setting, however, the
perspective is different: only 20% of patients receiving chemotherapy and
trastuzumab remain alive and progression-free at 3 years [1]. Therefore, events
are more frequent in the metastatic setting than in early-disease. In other
words, there is more room for improvement in metastatic disease, whereas in the
adjuvant setting chemotherapy and trastuzumab already yield high Disease-Free
Survival (DFS) rates.
Illustrating
this hypothesis, the addition of pertuzumab to trastuzumab and chemotherapy in
the metastatic setting yields a 32% relative reduction in the risk of
progression, which translates into an 8.2% absolute increase in
Progression-Free Survival (PFS) at 3 years, whereas in the adjuvant setting
pertuzumab yields a 24% relative reduction in the risk of recurrence at 6
years, translating into a modest 2.8% absolute improvement in invasive DFS
(iDFS) [1-3]. When considering only node-positive patients (who present a
higher risk of recurrence), the benefit of adjuvant pertuzumab becomes more
pronounced (28% relative reduction in recurrence risk yielding a 4.5% absolute
6-year iDFS improvement).
https://crimsonpublishers.com/smoaj/fulltext/SMOAJ.000560.php
Crimson
Publishers: https://crimsonpublishers.com/
For
more articles in Journal
of Surgical Medicine,
Please
click on below link: https://crimsonpublishers.com/smoaj/



No comments:
Post a Comment